Scaling Innovation: The Compounding Effects of Institutional Culture
Discover how human-centered design transforms communication in medicine, from personal mastery to institutional culture change.

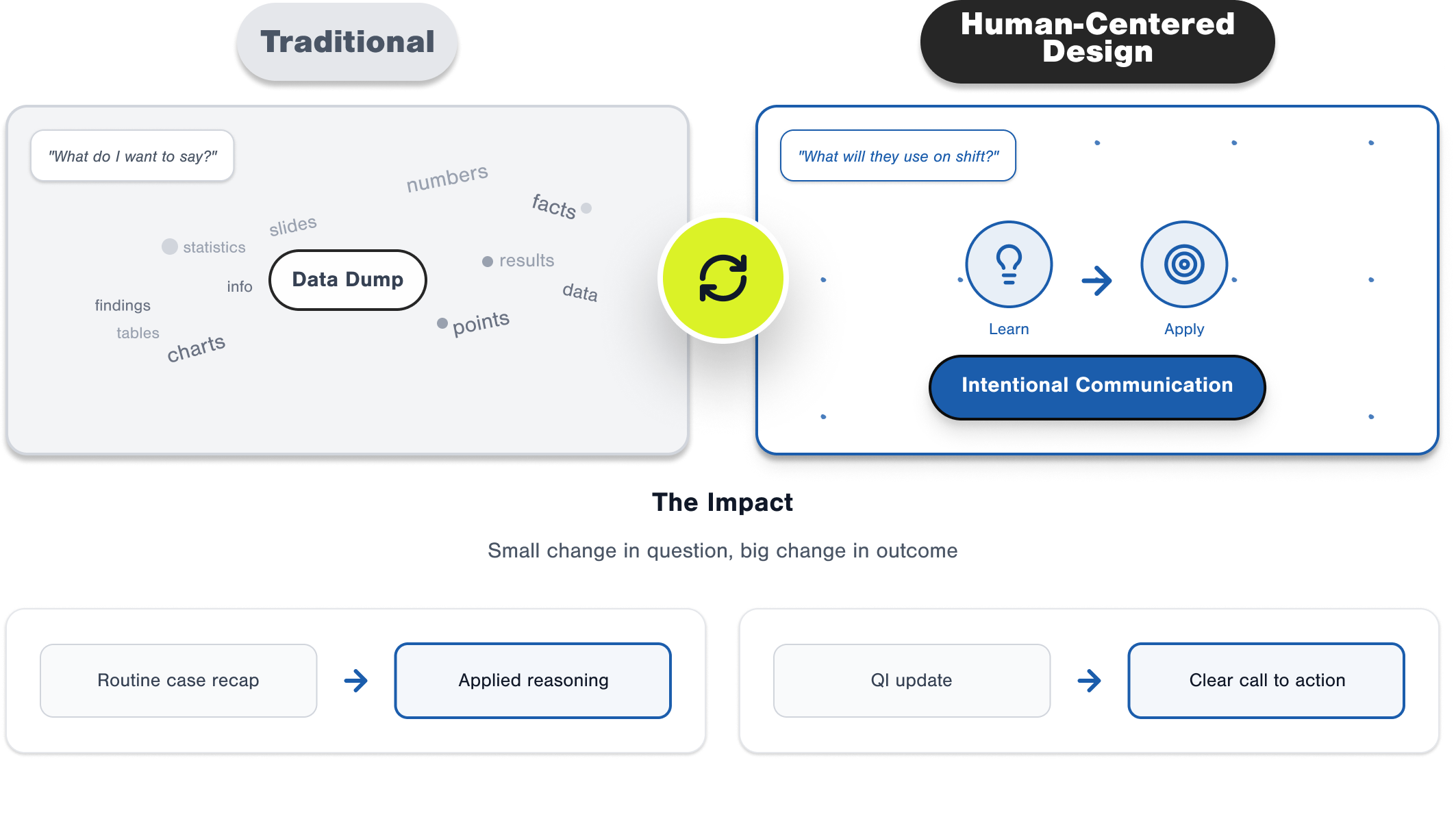
How Small Changes Spark Big Shifts
It started with one resident. Sitting in yet another M&M, frustrated by the endless march of labs and timestamps, she asked herself: "What do my colleagues actually need to take from this case so they practice differently tomorrow?" She reframed her talk around that question.
The difference was noticeable. Instead of glazed eyes, there were real conversations—attendings weighing in on how the system should change, residents debating diagnostic reasoning, nurses adding critical context. A case recap had turned into a learning moment. Within a few months, the department adopted new M&M templates. What began as one" experiment shifted how the entire department thought about presentations.
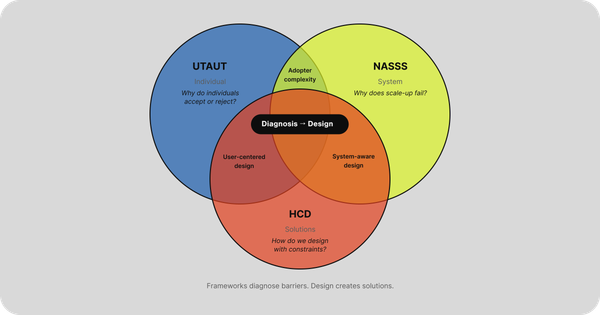
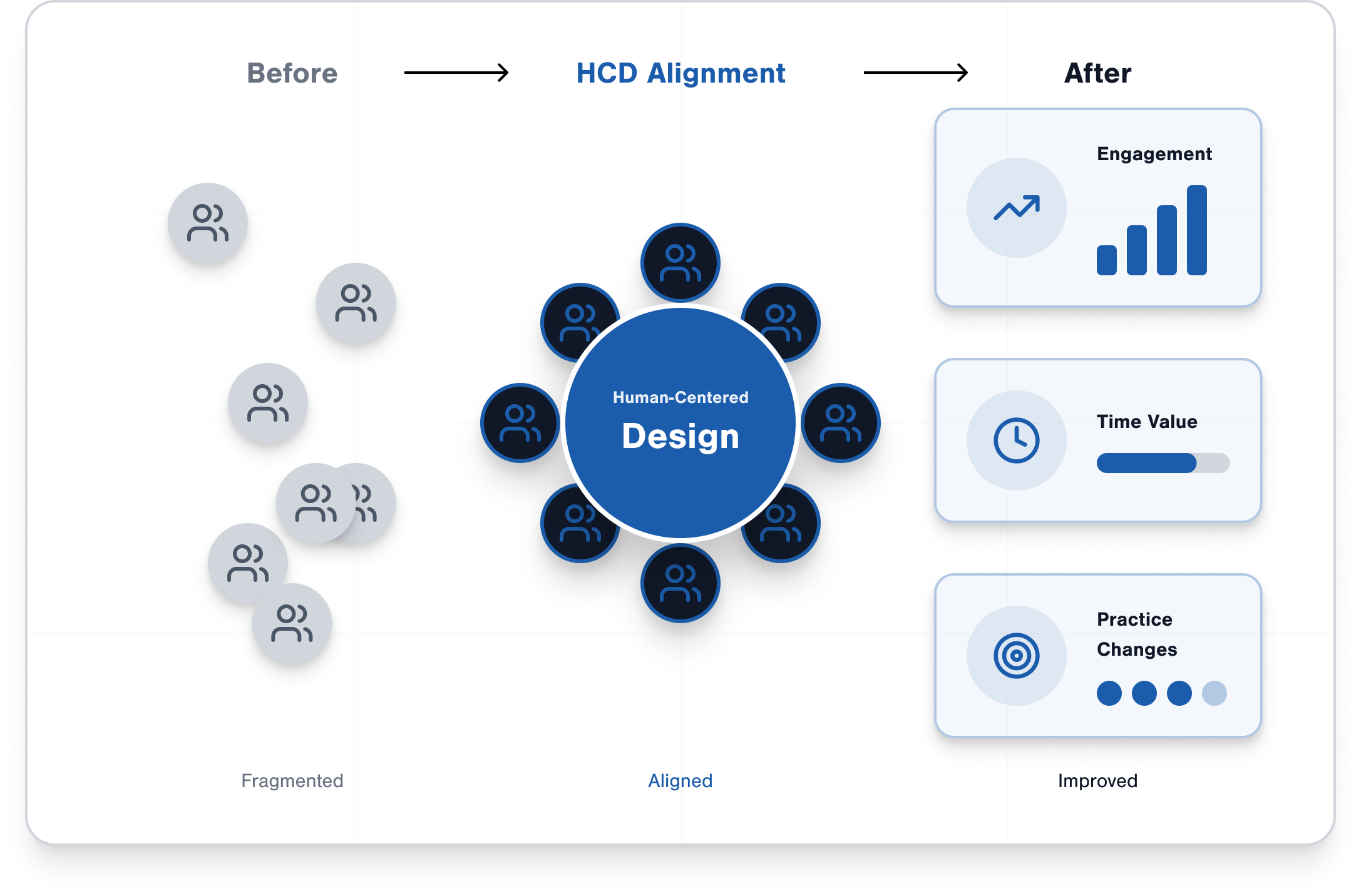
This is the power of human-centered design (HCD): not prettier slides, but a culture change grounded in designing communication for the people who use it. That spark of redesign at the individual level can cascade upward—first to departmental norms, and eventually to institutional culture.
Why Scaling Matters
As individuals, we've all hacked a presentation here or there—trimmed slides, restructured a case, tightened signouts. But in medicine, communication isn't cosmetic. It's life or death. The Joint Commission has consistently listed communication failures as a top cause of sentinel events (The Joint Commission, 2015). Every poorly structured talk, every bloated handoff, carries risk.
And then there's the time. Four hours of didactics = hundreds of clinician-hours. How often have we all sat in sessions that left us thinking, well, there's time that's not getting back? The hidden cost of poor communication is enormous.
HCD stops improvements from staying one-off. By starting with user needs, prototyping, and iterating with feedback, we create systems that scale. And maybe most importantly, HCD builds creative confidence. When people know the process values iteration over perfection, they feel safe to try new things. That's how cultures of continuous improvement start—first in a single session, then in how a department runs its conferences, and finally in how an institution approaches communication system-wide.
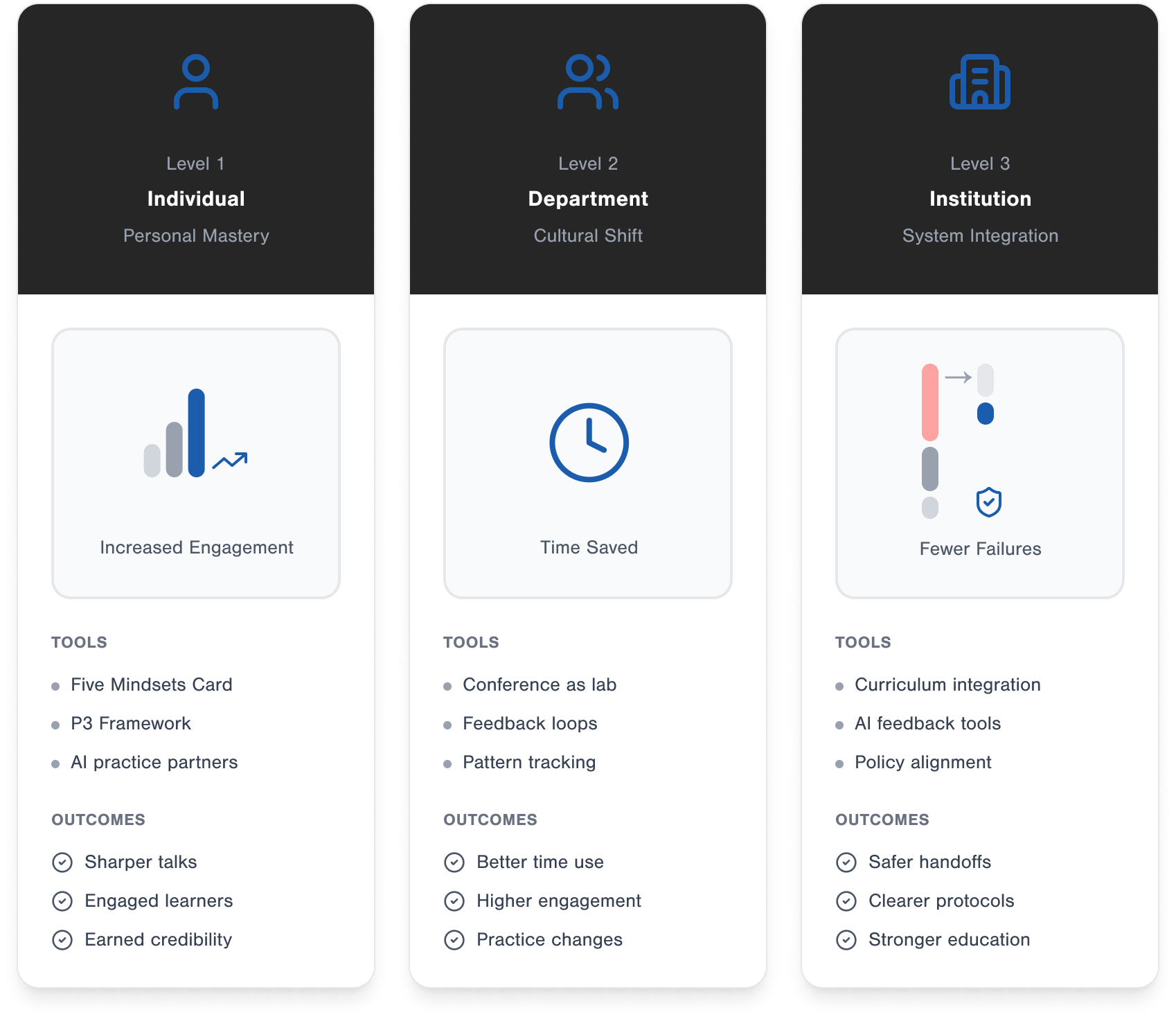
Three Levels of Implementation (through Human-Centered Design)
Level 1: Individual — Personal Communication Mastery
We've all asked ourselves before a talk: What do I want to say? HCD flips it: what does my audience need to learn, and how will they use it on shift? That small change turns a routine case recap into applied reasoning, or a QI update into an actual call to action.
Tools that help: the Five Mindsets Card, the P3 Framework Worksheet, and AI-assisted practice runs. They give clinicians a structure without piling on more work.
Outcomes: Talks feel sharper. People stay engaged. Learners walk away with something they can use. And the speaker earns credibility—not for flashy delivery, but for making everyone better.
Leadership perspective: This is faculty development without extra cost. Give people the right design tools and you get better educators without adding FTEs or budgets.
Culture link: Individual mastery plants seeds. When one resident reframes a case to highlight diagnostic reasoning instead of labs, it sets an example. Others borrow the approach. That's how individual design choices begin to shift norms.
Level 2: Department — Cultural Shift in EM
When a few individuals start designing this way, departments feel it. Conferences stop being endured and start being useful. M&M becomes about prevention, not blame. QI isn't just metrics; it's improvement. Didactics shift from content dumps to active learning.
Implementation through HCD:
- Templates built around "jobs to be done" (prevent error, adopt protocol, sharpen reasoning).
- Using conference time as a lab—prototype formats, iterate, refine.
- Build feedback loops into the structure so every conference improves the next.
Outcomes: Better use of time. Higher engagement. Real practice changes showing up after conference.
Leadership perspective: This is culture change. Instead of conference being a box to check, it becomes something people look forward to. You can measure ROI in engagement scores, evals, and even safety outcomes.
Culture link: At this level, culture change becomes visible. When every QI presentation highlights not just numbers but actions, or every M&M ends with a systems improvement, people expect it. Expectations shift. Norms evolve. That's the definition of departmental culture taking shape.
Level 3: Institution — Systematic Integration
At the institutional level, the question becomes: how do we make human-centered communication the norm rather than the exception?
Implementation through HCD:
- Build communication design into residency curriculum as a skill on par with procedures.
- Faculty workshops that train attendings to model it.
- AI-driven tools that give feedback on signouts or presentations in real time.
- Policies that make communication excellence part of competency milestones.
Outcomes: Safer handoffs. Clearer protocols between departments. Stronger medical education rooted in evidence and innovation. All reinforcing a culture that values clarity, continuous improvement, and safety.
Leadership perspective: This aligns perfectly with accreditation, risk management, and innovation goals. The hospitals that get this right don't just lead in med ed—they lead in patient safety and reputation.
Culture link: Once embedded in training, policy, and faculty expectations, communication design becomes part of the institution's DNA. New residents learn it from day one. Faculty model it automatically. Over time, HCD doesn't just change practice—it is the culture.
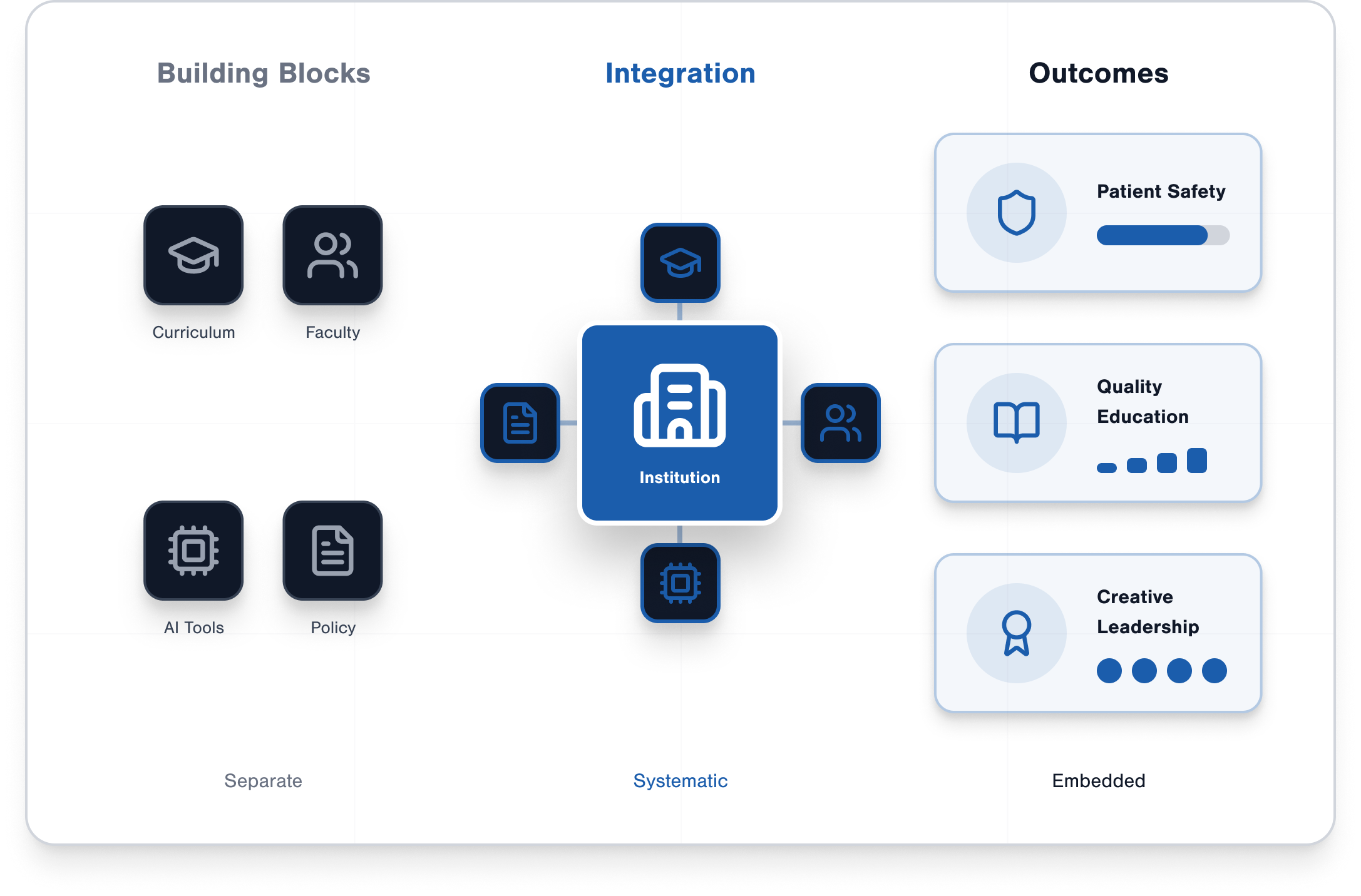
Putting It All Together
The multiplying effect happens when change is extrapolated across multiple dimensions of an institution. Others see the value of new problem-solving approaches, which generates greater buy-in. Over time, the value of human-centered design becomes embedded across the institution.
Overcoming Common Obstacles
"We don't have time." HCD actually saves time. Well-designed talks and handoffs are shorter, sharper, and more effective.
"Our audience expects tradition." Tradition" didn't give us clinical checklists or stroke alerts, either. Start small, evolve with feedback, and people adapt quickly when they see the value.
"This isn't evidence-based." It is. Narrative learning improves recall (Greenhalgh, 2001). Evidence-based teaching is the direction of higher ed (Groccia & Buskist, 2011). And communication failures are a known safety risk (The Joint Commission, 2015). HCD weaves these into a framework clinicians can actually use.
Change Agent Action Plan
- Start with one HCD-inspired redesign. This might mean taking your next M&M and structuring it around system change rather than a blow-by-blow case recap, or redesigning signouts so the receiver knows what actually to watch for.
- Find allies who see the impact. Share your approach with a co‑resident, nurse, or attending who will back you up. Small groups make it easier to sustain momentum.
- Document outcomes (engagement, clarity, adoption). Track how many questions your session generated, whether residents repeated back the key learning point, or if your team actually changed a protocol afterward.
- Scale stepwise: one session → department → institution. Once you've shown proof of concept, pitch the idea of standardized templates or workshops at the departmental level. If those stick, advocate for inclusion in residency curriculum or faculty development.
- Use the Change Agent Worksheet to guide the process. The worksheet walks you through each step and keeps you focused on iterating instead of trying to overhaul everything at once.
Conclusion + Series Wrap
We started this series by naming the problem: medical presentations are broken. Along the way, we explored design mindsets, the P3 framework, and now the path to scaling change.
The core truth is this: communication you've extra—it is patient care. When we design our communication with the same rigor we bring to protocols and procedures, we change not just talks, but departments and institutions.
Your next step: try one HCD-inspired change. See what happens. Build from there. That's how cultures shift—from individuals, to departments, to entire institutions.
📥 Download the Change Agent Action Plan to carry this work forward.
Greenhalgh, T. (2001). Narrative based medicine: Narrative based medicine in an evidence based world. BMJ, 323(7318), 323–325. https://pmc.ncbi.nlm.nih.gov/articles/PMC1114786/
Groccia, J. E., & Buskist, W. (2011). The need for evidence-based teaching. New Directions for Teaching and Learning, 2011(128), 5–11. https://mclaughlinannotatedbibarticles.weebly.com/uploads/1/9/3/2/19328259/need_for_evidence-based_teaching.pdf
The Joint Commission. (2015). Root causes of sentinel events. Sentinel Event Data Root Causes Report. Retrieved from https://www.jointcommission.org/en-us/knowledge-library/sentinel-events